Diagnosing and treating blood cancers
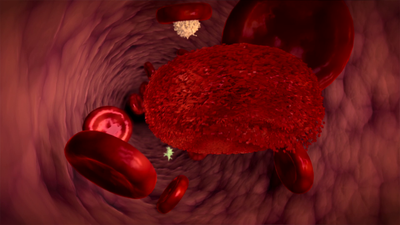
A complete blood count is a basic blood test to determine the patient's health. It allows for the detection of infections, inflammations and shortages or excesses of particular types of blood cells, which may indicate a developing blood cancer.
Unveiling Blood Cancers: The Power of Early Detection
An early-stage complete blood count (CBC) provides initial hints about blood cancers. It evaluates red blood cells, white blood cells, and platelets. Abnormalities in these cell counts may suggest developing blood cancers like acute lymphoblastic leukemia (ALL), chronic lymphocytic leukemia (CLL), acute myeloid leukemia (AML), or chronic myeloid leukemia (CML). This may sometimes lead to the detection of other blood disorders:
- Low platelet count (thrombocytopenia)
- High red blood cell count (polycythemia)
- Lymphomas like Hodgkin lymphoma and non-Hodgkin lymphoma
- Myelomas like multiple myeloma
- Primary myelofibrosis
Despite the fact that CBC is the first step in diagnosing blood cancers, it is imperative to do more advanced diagnostic tests.
Beyond the CBC: Advanced Diagnostic Techniques
Bone marrow biopsy
A bone marrow biopsy is a standard diagnostic test. Two forms of this biopsy exist: fine-needle aspiration biopsy and percutaneous trepan biopsy. It involves taking a small sample of bone marrow tissue for evaluation with a microscope to assess for abnormalities in blood cell production.
Molecular and cytogenetic tests
Molecular tests
Molecular tests use techniques like FISH (Fluorescence in situ hybridization) and PCR to identify gene locations and mutations, enhancing our understanding of diseases such as leukemia. Such tests provide valuable insights into the genetic makeup of cancer cells, which aids personalized treatment approaches.
Cytogenetic testing
By analyzing the structural and functional nature of chromosomes, cytogenetic testing is a comprehensive diagnostic tool for leukemia. It identifies chromosome abnormalities and the karyotype, essential in being able to understand the genetic makeup of this disease.
Standard therapies - radiotherapy and chemotherapy
Chemotherapy
Most chemotherapy drugs are drugs designed to target the division of cells that are rapidly multiplying; thus, for cancer cells, it may eliminate the disease or, in some cases, be only symptomatic. The side effects of chemotherapy can include hair loss, nausea, and fatigue, all of which can be managed with supportive care.
Stem cell transplantation
Stem cell transplantation is an avenue that carries hope for patients with leukemia and other blood diseases. Preparation and transplantation of stem cells is a complex procedure aimed at replacing the patient's damaged bone marrow. In allogeneic transplantation, the transplant recipient requires a compatible donor, whereas autologous transplantation employs the patient's cells, each with its pros and cons. Despite the fact that stem cell transplantation carries a number of challenges, it has considerably improved survival outcomes in patients afflicted with leukemia and other blood disorders, offering a possible cure for those that fail other available treatments.
Transplantation of bone marrow from a related or unrelated donor
The transplantation process begins with pre-qualification that includes an evaluation of the candidate suitability for transplantation and the assessment of associated risks at the transplant center. Next, a comprehensive patient examination follows, assessing organ capacity and excluding potential risk factors. It is a step to gain optimal outcomes for the transplantation and post-transplantation phases. Then, donor search starts, looking for HLA-matched donors first within the family. Only around 30% of patients manage to find a matching family donor. On top of that, even family donors may be ineligible due to reasons concerning health, so the search for an unrelated donor is intensified worldwide, including, but not limited to, stem cell registries. Eligible persons aged 18 to 55 and healthy can register with DKMS as potential blood stem cell donors, with exclusions based on chronic, genetic, autoimmune, or infectious diseases. Between 80% to 90% of Polish patients get an unrelated donor.
Conditioning before transplantation is preparation that involves chemotherapy and possibly radiotherapy to eradicate cancer cells. Unfortunately, it also pushes away normal bone marrow, and blood stem cell transplantation has to be in place in order to rebuild it. This may lead to temporary decreases in key blood parameters—white blood cells, platelets, and red blood cells—that demand transfusions with donated blood.
The transplantation procedure consists in transferring donor hematopoietic stem cells into the patient’s body. It is a simple blood transfusion that lasts a few minutes to one hour. Typically, 80% of the transplanted material is derived from the peripheral blood, while 20% is derived from the pelvic bone. Following the transplantation procedure, the engraftment, known as the post-transplantation phase, starts. The fact that after 14 to 30 days new white blood cells are detected in peripheral blood ensures success of the transplantation and functionality of bone marrow, thus making more complex the demand for further transfusions of blood.
At this moment, the patient's immune system is weakened during waiting, creating infections and complications as they are very weak, thus always necessitating inspection at all times. In order to avoid infection, stringent protocols and regulations are placed. In spite of these severe restrictions, there have been minor infections that need immediate attention. While waiting for engraftment, patients may experience bone and joint pain due to the gastrointestinal mucosa. However, as new blood cells are emerging, the condition of the patients dramatically improves. When stable conditions with sufficient normal blood cells are reached, then the patient can be discharged. Typically, weekly check-ups and potential red blood cell transfusions are carried out at the transplant center..
Autologous blood stem cell transplantation
In this case, the patient is both a recipient and a donor of blood stem cells. The patient's remission of the disease is induced and during that time hematopoietic blood stem cells are collected and frozen. After some time, conditioning, i.e. preparation of the patient with high-dose chemotherapy and/or whole-body radiation, is carried out. The next step is to transplant the patient with their own, frozen blood stem cells, which are used to regenerate blood.
Autologous transplantation has no anticancer effect, which results from the activity of immune cells. It is also not associated with such a high risk of complications, as in the case of transplantation from related or unrelated donors.
Hematopoietic blood stem cell transplantation is a method that gives them hope of a cure for many blood diseases. It improves the prognosis in certain types of leukemia. It is a complicated process and burdensome for the patient's body, but this method also gives a chance to be cured of a serious disease.
Register now to save a life! Your simple act of registering as a potential blood stem cell donor could offer hope to someone in need. Click below to sign up and make a difference today.